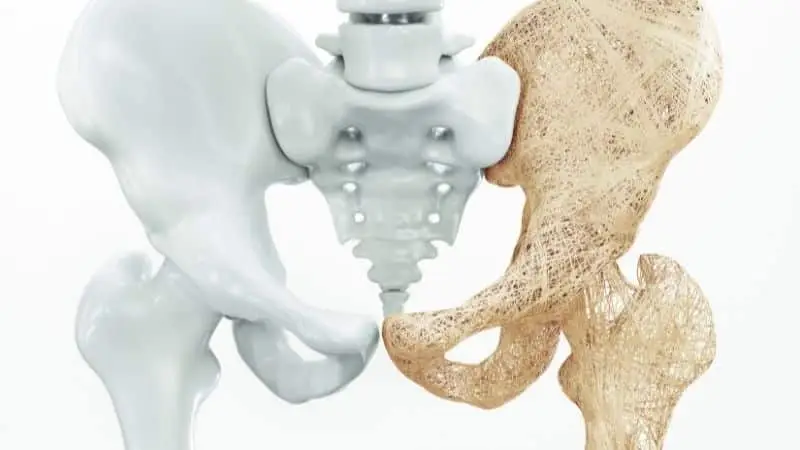
What Is Osteoporosis:
Osteoporosis, or “porous bone”, is a common bone disease characterized by low bone mass density (thickness of the bone), decreased bone strength, and a change (deterioration) in the bone structure and tissue, which can lead to an increased risk of fracture.
The normal bone structure becomes thinned out, brittle, and porous, lessening the ability of the bone to withstand the typical forces that are applied in everyday living. Fractures from osteoporosis and low bone density can be serious, causing pain and affecting your quality of life.
It also can lead to changes in posture, and an increased susceptibility to fractures, especially of the hip, spine, and wrist. While Osteoporosis and Osteopenia are both a result of a decrease in bone density, Osteopenia is a less severe form of osteoporosis.
In this blog post, we will go into more detail about who is at risk, and what can be done about it. To schedule a complimentary screening, please fill out this form.
Who Is At Risk:
Postmenopausal women ages 45-55 have the highest risk, due to a decrease in estrogen are at risk for the weakening of bones.
However, it can also occur in men and in children, often due to diseases that affect bone development, such as Celiac disease, inflammatory bowel disease, rheumatoid arthritis, spina bifida, cystic fibrosis, or kidney disease.
Some medicines, such as steroids, may increase your risk for developing osteoporosis. Athletes who are underweight during the time of peak bone development are also susceptible. Some risks include:
- A small thin frame
- Alcoholism
- Sedentary lifestyle
- Family History
- Low calcium intake
- Predisposing medical conditions
- Cigarette smoking
- Excessive alcohol intake
- Inactive lifestyle
- Excessive caffeine intake
- Lack of weight-bearing exercise
- Poor health
- Low weight
- Calcium-poor diet
- Low vitamin D levels
How Common Is Osteoporosis:
A panel of experts judged that skeletal fragility might be responsible for 80–95 percent of hip and spine fractures in women, depending on age, along with 70–80 percent of distal forearm fractures and 45–60 percent of fractures at other skeletal sites (Melton et al. 1997).
Roughly 40% of women 50 or older in the US will experience a hip, spine or wrist fracture during their life. (National Osteoporosis Foundation)
Roughly one in four (24 percent) women age 50 or older fall each year, compared to nearly half (48 percent) of women age 85 or older; comparable figures for men are 16 percent and 35 percent (Winner et al. 1989).
One in 4 women will develop osteoporosis in her lifetime. A woman’s risk of having an osteoporosis-related hip fracture is greater than her risk of developing breast, uterine, and ovarian cancer combined. (National Osteoporosis Foundation)
How It Is Diagnosed:
Osteoporosis is best diagnosed through a quick and painless specialized x-ray called the DXA, which measures bone density. The results are reported using T-scores and Z-scores.
The T-score compares your score to that of healthy 30-year-old adults. If you have a T-score of -1 or less, you have a greater risk of having a fracture.
The Z-score compares your bone mineral density to those of the same sex, weight, and age. It is used for those whose bone mass has not yet peaked, premenopausal women, and men older than 50.
Other methods of measuring bone density include x-ray, ultrasound, and CT scan.
Osteoporosis Prevention
While no one can guarantee any preventative action will be 100% successful, it sure doesn’t hurt! So what can you do? After being cleared by a Medical Professional, try:
Walking
It is recommended that you walk 45 minutes a day at least 4 days a week.
Balance Training
1 legged standing for one minute is equivalent to the amount of integral load gained through walking for approximately 53 minutes. (Sakamoto, 2006)
Body Weight Training
12 weeks of squatting 3 times a week improved skeletal properties in postmenopausal women with osteopenia or osteoporosis. (Mosti, 2013)
How a Physical Therapist Can Help:
Your physical therapist can develop a specific program based on your individual needs to help improve your overall bone health, keep your bones healthy, and help you avoid fracture. Your physical therapist may teach you:
- Specific exercises to build bone or decrease the amount of bone loss
- Proper posture
- How to improve your balance so as to reduce your risk of falling
- How to adjust your environment to protect your bone health
Healthy bone is built and maintained through a healthy lifestyle. Your physical therapist will teach specific exercises to meet your particular needs.
The exercise component for bone-building or slowing bone loss is very specific and similar for all ages.
Bone grows when it is sufficiently and properly stressed, just as a muscle grows when challenged by more than usual weight. Two types of exercise are optimal for bone health, weight-bearing and resistance.
It is best for a physical therapist to provide your individual bone-building prescription to ensure that you are neither over- or under-exercising. Typically, exercises are performed 2 to 3 times a week as part of an overall fitness program.
If you or anyone you know is suffering from Osteoporosis, feel free to give us a call or schedule an Initial Examination with our world-class Physical Therapists.
Natural Treatment Alternatives
Osteoporosis is not solely caused by a dietary calcium deficiency, therefore simply taking calcium supplements will NOT remedy the problem.
The problem is either not enough absorption of calcium into the bones or a loss of existing calcium from the bones of our body.
So, what are some dietary changes we can make or natural supplementation we can take to help combat bone mass loss?
Dietary Changes
Let’s start with foods that help maintain healthy calcium levels. Vitamins C, D, E, and K plus the mineral’s silicon, magnesium, phosphorus, boron, zinc, manganese, and copper are helpful. Amino acids and fatty acids are also important in maintaining proper calcium.
Many experts agree our body’s pH level may also be a significant contribution to osteoporosis. When pH in our body drops to just 7.38, the body begins to break down bone and muscle tissues to use their alkalizing ammonia, carbonate, and phosphates.
Bones serve not only as our support structure, they also serve as the storage facility for acid-neutralizing minerals.
Diets high in animal protein, such as fish, meat, and cheese are acid-producing foods. Researchers found that women who were eating a high acid-producing diet had more rapid bone loss and 3.7 times greater risk of hip fracture than women eating fewer acid-producing foods.
Intake of foods high in oxalic acid – almonds, chard, asparagus, beet greens, cashews, rhubarb, and spinach tend to inhibit calcium absorption by creating an acid environment. Also avoid dark colas, alcoholic drinks, coffee, and caffeinated drinks.
Alkalizing Foods
So, what are some alkalizing foods?
all vegetables and fruits (except blueberries, plums, prunes, and cranberries) are alkalizing. Even citrus fruits such as lemons, which we think of as being acidic, are alkaline-producing in the body.
Beans, such as string, soy, lima, green, and snap peas are alkalizing. Eggs, milk, cream, whey, plain yogurt, potatoes, grains, nuts, and many spices are alkaline-producing.
The best balance is 70% alkaline and 30% acid. The normal range of saliva pH is 6.5 to 7.0 and is easy to test with litmus strips.
Absorption
An important component of taking calcium supplements is absorption. There must be an adequate supply of vitamin D as well as sufficient Hydrochloric (HCL) Acid in the stomach.
Frequently, people over the age of 55 lack sufficient stomach acid and therefore should select a calcium supplement that contains the digestive acid Betaine Hydrochloride, additional magnesium, and vitamin D.
Hormone Deficiencies
Lastly, hormone deficiencies are a cause of low calcium levels.
Studies have looked at different hormone replacement therapies resulting in a reduced rate of bone turnover using Estradiol and oral progesterone (Norgestimate).
Natural progesterone creams, which have shown similar results, are a good alternative to the side effects associated with progestins, which are chemically altered or synthetic forms of progesterone.
So, when considering treatment for osteoporosis or trying to prevent it, realize that there are many natural, safe alternatives you can take advantage of. Consult your physician or physical therapist for more information.
If after reading this article you have any concerns or think you might be at risk, please come in for a complimentary wellness screening.